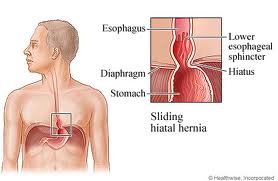
According to the information and definition by Mayo Clinic, it states that a hiatal hernia occurs when part of your stomach pushes upward through your diaphragm. Your diaphragm normally has a small opening (hiatus) that allows your food tube (esophagus) to pass through on its way to connect to your stomach. The stomach can push up through this opening and cause a hiatal hernia.
*
*
In most cases, a small hiatal hernia doesn't cause problems, and you may never know you have a hiatal hernia unless your doctor discovers it when checking for another condition. But a large hiatal hernia can allow food and acid to back up into your esophagus, leading to heartburn and chest pain. Self-care measures or medications can usually relieve these symptoms, although a very large hiatal hernia sometimes requires surgery.
Symptoms
Symptoms
Most small hiatal hernias will cause no signs or symptoms. But, the larger hiatal hernias can cause signs and symptoms such as :
A hiatal hernia occurs when weakened muscle tissue allows your stomach to bulge up through your diaphragm. It's not always clear why this happens, but pressure on your stomach may contribute to the formation of hiatal hernia.
*
*
How a hiatal hernia forms
Your diaphragm is a large dome-shaped muscle that separates your chest cavity from your abdomen. Normally, your esophagus passes into your stomach through an opening in the diaphragm called the hiatus. Hiatal hernias occur when the muscle tissue surrounding this opening becomes weak, and the upper part of your stomach bulges up through the diaphragm into your chest cavity.
*
Your diaphragm is a large dome-shaped muscle that separates your chest cavity from your abdomen. Normally, your esophagus passes into your stomach through an opening in the diaphragm called the hiatus. Hiatal hernias occur when the muscle tissue surrounding this opening becomes weak, and the upper part of your stomach bulges up through the diaphragm into your chest cavity.
*
Possible causes of hiatal hernia
- Injury to the area
- An inherited weakness in the surrounding muscles
- Being born with an unusually large hiatus
- Persistent and intense pressure on the surrounding muscles, such as when coughing, vomiting, or straining during a bowel movement or while lifting heavy objects
This sort of complication occurs commonly in people who are :
- Age 50, or older
- Obese
- Smokers
If you've been diagnosed with a hiatal hernia and are experiencing signs and symptoms that aren't controlled with medications and lifestyle changes, ask your doctor for a referral to a doctor who specializes in digestive diseases (gastroenterologist).
A hiatal hernia is often discovered during a test or procedure to determine the cause of heartburn or chest or upper abdominal pain, such as :
- An X-ray of your upper digestive tract. During a barium X-ray, you drink a chalky liquid containing barium that coats your upper digestive tract. This provides a clear silhouette of your esophagus, stomach and the upper part of your small intestine (duodenum) on an X-ray.
*
- Using a scope to see inside your digestive tract. During an endoscopy exam, your doctor passes a thin, flexible tube equipped with a light and video camera (endoscope) down your throat and into your esophagus and stomach to check for inflammation.
Treatments and drugs
Most people with hiatal hernia don't experience any signs or symptoms, and won't need treatment. If you experience signs and symptoms, such as recurrent heartburn and acid reflux, you may require treatment, which can include medications or surgery.
*
*
Medications for heartburn
If you experience heartburn and acid reflux, your doctor may recommend medications, such as :
If you experience heartburn and acid reflux, your doctor may recommend medications, such as :
- Antacids that neutralize stomach acid. Over-the-counter antacids, such as Maalox, Mylanta, Gelusil, Rolaids and Tums, may provide quick relief. But antacids alone won't heal an inflamed esophagus damaged by stomach acid. Overuse of some antacids can cause side effects, such as diarrhea or constipation.
*
- Medications to reduce acid production. Called H-2-receptor blockers, these medications include cimetidine (Tagamet HB), famotidine (Pepcid AC), nizatidine (Axid AR) or ranitidine (Zantac 75). H-2-receptor blockers don't act as quickly as antacids, but they provide longer relief. Stronger versions of these medications are available in prescription form.
*
- Medications that block acid production and heal the esophagus. Proton pump inhibitors block acid production and allow time for damaged esophageal tissue to heal. Over-the-counter proton pump inhibitors include lansoprazole (Prevacid 24HR) and omeprazole (Prilosec OTC). Stronger versions of these medications are available in prescription form.
Surgery to repair a hiatal hernia
In a small number of cases, a hiatal hernia may require surgery. Surgery is generally reserved for emergency situations and for people who aren't helped by medications to relieve heartburn and acid reflux. Hiatal hernia repair surgery is often combined with surgery for gastroesophageal reflux disease.
In a small number of cases, a hiatal hernia may require surgery. Surgery is generally reserved for emergency situations and for people who aren't helped by medications to relieve heartburn and acid reflux. Hiatal hernia repair surgery is often combined with surgery for gastroesophageal reflux disease.
An operation for a hiatal hernia may involve pulling your stomach down into your abdomen and making the opening in your diaphragm smaller, reconstructing a weak esophageal sphincter, or removal of the hernia sac. In some cases, this is done using a single incision in your chest wall (thoracotomy) or abdomen (laparotomy). In other cases, your surgeon may insert a tiny camera and special surgical tools through several small incisions in your abdomen. The operation is then performed while your surgeon views images from inside your body that are displayed on a video monitor (laparoscopic surgery).
Lifestyle changes may help control the signs and symptoms of acid reflux caused by a hiatal hernia. Consider trying to :
- Eat several smaller meals throughout the day rather than a few large meals.
- Avoid foods that trigger heartburn, such as chocolate, onions, spicy foods, citrus fruits and tomato-based foods.
- Avoid alcohol.
- Limit the amount of fatty foods you eat.
- Sit up after you eat, rather than taking a nap or lying down.
- Eat at least three hours before bedtime.
- Lose weight if you're overweight or obese.
- Stop smoking.
- Elevate the head of your bed 6 inches (about 15 centimeters).
- Work to reduce the stress in your daily life.



No comments:
Post a Comment