[Extracted from www.vascular.co.nz]
An angioplasty is a procedure where a balloon is passed into your artery on the end of a tube (catheter) and is inflated (blown up) to treat a narrowed or blocked artery. The initiator of this technique was Charles Dotter, a radiologist in Oregon who started this work in 1964. The angioplasty technique means that surgery may be avoided in many cases. There are two techniques for performing angioplasty - transluminal and subintimal. In the transluminal technique the balloon is placed in the centre of the artery (in the lumen) where blood would normally flow.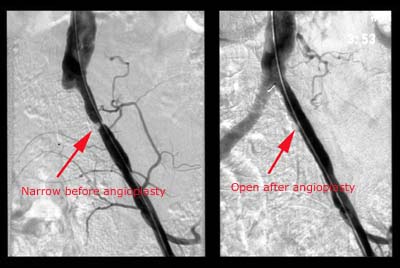
In subintimal angioplasty (Bolia, 1989) the balloon is intentionally placed within the layers of the arterial wall. As far as the patient is concerned, angioplasty is very similar to an angiogram except that a slightly bigger catheter is used and therefore the risks of bleeding are slightly greater. For this reason, in most cases, you will be asked to stay overnight. You will usually be asked to start taking aspirin before you are admitted as this makes the blood less sticky. A common dose is 75 mg per day. If you have a stomach ulcer or are allergic to aspirin, please tell your doctor.The angiogram opposite shows the artery on the left before angioplasty and on the right following angioplasty.
Angioplasty takes a little longer than simple angiography and you may feel the doctor changing, and pushing, catheters in and out of your groin artery. Although this is occasionally a little uncomfortable, it is not usually too painful. Once in position the artery will be stretched by inlating the balloon. This is a special balloon (Gruentzig balloon) that will only inflate to a fixed diameter which will vary depending on the size of the artery being treated. The reason for this is that the fixed diameter prevents overinflation of the balloon and reduces the risk of rupturing the artery. If there appears to be a good angiographic result no further procedures may be necessary. Sometimes, if the appearance of the treated artery is not ideal the situation can be improved or salvaged by inserting a special device called a stent to keep the artery open. This is just a small metal tube that expands in your artery to keep the area open and allow more blood to flow through. Stents appear to be especially useful in larger arteries above the level of the hip joint.
They can be used in arteries in the thigh but results are mixed and it should not be a routine procedure at this level of the leg. An editorial in the British Journal of Surgery recently concluded that "doctors have not the slightest clue whether primary stenting for arterial occlusive disease below the inguinal ligament (groin area) is of any real use" (Reekers 2008).
Unless there is a contraindication most patients should be taking aspirin. In some cases Heparin injections (anticoagulation) will be given for 24 hours to prevent the blood clotting at the site of the angioplasty. Rarely you may require warfarin tablets to thin the blood for a few months. You will normally be allowed home the following day. If you are given heparin or warfarin this may delay your departure by a few days. There is a growing trend to use clopidogrel to improve angioplasty success in leg arteries as it does seem to be important in patients undergoing coronary angioplasty in the heart. There is no evidence that clopidogrel is helpful following lower limb angioplasty.
You will be seen again in the clinic by your surgeon to assess the success of the angioplasty and to decide upon any further treatments. Unfortunately, in about 10% of cases, angioplasty is not successful and other treatments will need to be considered. In addition, even where successful angioplasty has been performed, there is a risk that the area in the artery will narrow down again. After one year, about 20-40% of arteries will have re-narrowed. In some cases, it may be possible to repeat the angioplasty at that time although in others this may not be possible. Very rarely, if angioplasty does not work, the circulation may actually worsen. If this is a particular risk in your case, your surgeon and /or radiologist will discuss the risks with you.
What are the possible side effects/complications ?
False aneurysm - rarely a pulsating lump develops in the groin at the site where the catheter was inserted into the artery. This is because bleeding took place after the catheter was removed. The clot produced forms a small sac with liquid blood in the centre. This blood pulses because it is connected to the artery through the hole made by the catheter. The sac with blood in the centre is called a false aneurysm. These days this problem can usually be treated by a simple injection into the sac to make the liquid blood in the centre form a clot and block the small hole in the artery. Thrombin is the naturally occurring blood clotting agent which is injected. It is usually very effective.
Pain/Discomfort – local anaesthetic is injected into the skin just before the catheter is placed into the artery. This should take away any severe pain, but it is likely you may feel some gentle pushing and pulling during the procedure. The blood vessels themselves do not feel the guiding wire or catheter. Injecting the dye sometimes causes a sensation of warmth, but this usually lasts only a few seconds.
Reactions to the dye – Reactions to modern dyes apart from the sensation of warmth are very uncommon. Various reactions and allergies can still occur and the staff are fuly trained and equipped to deal with any reaction which may occur. Reactions may include skin rashes, vomiting, asthma, low blood pressure and disturbances of heart beat and kidney damage. Kidney damage is a real risk but only inpatients with kidney function already impaired. If your kidney function is normal no special precautions are required. If your kidney function is abnormal then patients are routinely given intravenous fluids for some hours before the procedure. This not only dilutes the dye as it passes through the kidneys but also acclelerates the passage of dye throught the kidney lessening the risk of damage. Other treatments have been tried to reduce kidney injury but there is no evidence they are effective.
Damage to blood vessels – this can occur during angioplasty especially if the artery is already badly diseased. The catheter may make a hole in the blood vessel or strip the lining from the blood vessel. Usually these problems can be dealt with by the radiologist at the time of the procedure. If it is not possible to deal with the problem in radiology then an operation may be required.
Nerve effects– sometimes the local anaesthetic can numb main nerves in the front of the thigh, causing numbness going down the leg and weakness. This will wear off after an hour or so.
Equipment failure – it is theoretically possible for the catheter or its guiding wire to break and leave a fragment inside the body. Procedures are available to deal with this eventuality in the radiology department but occasionally surgery may be required. Failure of technique – occasionally it is not possible to perform the angioplasty. This may be because the artery is too diseased. Sometimes inserting a metal stent to hold the artery open can be helpful, especially for larger arteries in the pelvis.
Blood clots – blood clots can form at the angioplasty site within the artery. These can usually be dealt with by using enzymes that dissolve the lot, but can sometimes be a problem which can cause the circulation to deteriorate.
Kidney damage - Damage can occur to cells in the kidney during an angiogram. This can lead to a deterioration in kidney function if your kidneys are already diseased. The cause of the damage is the special radio-opaque dye that is injected into the arteries so that they can be seen with X-rays. Although other dyes are available (gadolinium) they are probably no safer than conventional dyes. If the doctors know your kidneys may be at risk during an angiogram, they can reduce the risks of damage by giving extra fluids in an intravenous drip before during and after your angiogram.
Can I do anything to help myself ?
You cannot do anything to relieve the actual narrowing in your arteries. However, you can improve your general health by taking regular exercise, stopping smoking and reducing the fat in your diet. Your blood pressure should also be measured and kept under control. These actions will help slow down the hardening of the arteries which caused the problem in the first place, and may avoid the need for further treatment in the future.
How effective is angioplasty ?
The effectiveness of angioplasty depends on exactly which type of angioplasty is performed. In general if the artery is only narrowed, and has not totally blocked, then angioplasty is more likely to be successful and any improvement is likely to last longer. If the length of artery to be treated is short (less than 5cms), then angioplasty is likely to be more successful than if a much longer length of artery is diseased and requires treatment. Angioplasty is more likely to be successful in a large artery (iliac arteries in pelvis) versus a small artery (tibial arteries in calf). Other factors that may be important are the amount of plaque and degree of calcification present. Disease at the origin or start of a blood vessel when it branches may jeopardise success. Apart from technical issues related to the angioplasty, factors such as diabetes and thrombophilia are important in ongoing benefits from angioplasty.
A 1 cm long narrowing in a large iliac artery (in the pelvis) supplying the leg, treated by angioplasty is likely to produce a very good result. In contrast a 10cms blockage in a tibial artery in the calf may be very tricky to treat by angioplasty. Overall angioplasty is technically successful in 90-100% of patients, but the late results can be less impressive. For short arterial occlusions in the thigh the angioplasty site can remain open in 60-80% of patients, but the effect on symptoms is frequently poorly investigated. In less suitable arterial disease the benefits of angioplasty may be considerably less. In a study reporting the results of subintimal angioplasty for severe arterial disease in the legs only 25% (25 in 100) of the arteries were still open at 12 months and results were poorer when segments of artery greater than 10cms long were treated (Smith BM et al, 2005). The patency rates (whether the artery is open or not) of angioplasty are important, but what matters to the patient is whether their quality of life is improved. For instance a patent artery after angioplasty may improve walking distance by 100 metres, but the patient may feel almost as much disability as they did before their angioplasty. If the angioplasty does not improve quality of life and decrease the disability suffered by the patient it is worthless, even if the artery is open and the patient can walk a little further on a treadmill. There is some evidence that angioplasty makes minimal difference to quality of life particularly over the longer term (Spronk et al 2008).
A recent study (BASIL, 2005) has compared angioplasty with bypass surgery in patients with severe limb ischaemia (see bypass surgery). In patients who are suitable for both angioplasty and bypass surgery, an angioplasty first strategy had broadly similar outcomes to surgery, although a more recent analysis indicates surgery is a more durable policy in patients with a life expectancy of more than 2 years. Unfortunately, the majority of patients presenting with severe disease (approximately 80%) are not suitable for both strategies and are more likely to require surgery. In general vascular specialists will attempt angioplasty first in place of surgery if there is a reasonable chance of a good outcome. If this fails bypass surgery is still likely to be an option. In the USA, since 1996, there has been a 40% increase in the use of angioplasty in the leg arteries and a 30% decline in open bypass surgery (Nowygrod, 2006).
Other techniques
Cutting balloon angioplasty (using blades on the external balloon surface to score the inside of the artery), laser assisted angioplasty (cutting through and vapourising plaque with a laser), cryoplasty (using freezing) and mechanical devices to remove plaque have all been tried and found wanting in terms of patency rates and superiority over simple balloon angioplasty.






No comments:
Post a Comment